PERT Project
Collaborators
Norrlands University Hospital
Expertise
Design Research
Experience Design
Sector
Healthcare
Date
June 2010 - June 2013
Challenge
Adults with cancer often experience fear and worry about their disease. If they undergo radiotherapy, these emotions can be greatly exacerbated by the immobilization technologies used to accurately position and target their cancer with radiation.
These technologies are well known to cause anxiety and claustrophobia in patients, and can impact patients’ quality of life during treatment. Not only can interactions with the immobilization technologies unintentionally trigger patient anxiety, but this anxiety can lead to a decrease in efficacy of radiotherapy.
“It was my aim in this project to investigate why radiotherapy technologies cause strong negative emotional responses in patients, and how design might be used to alleviate or eliminate the sources of these emotions.”
Role
In this project, I planned and executed research within the Radiotherapy Department of Norrlands University Hospital to understand the adult cancer patient’s experience of radiotherapy treatment. I implemented a mixed-methods approach, comprised of qualitative, quantitative, and design methods. Through synthesis of my research findings, I identified key pain points and design opportunities within the treatment process. Working in close collaboration with nursing researchers and the radiotherapy care staff, I developed and tested two experience design prototypes aimed at decreasing patient anxiety caused by the immobilization technologies
Process
Ethnographic Fieldwork
I conducted ethnographic fieldwork on site within the Radiotherapy Department, observing over 50 patients and 30 staff members. I also conducted informal interviews with 12 radiotherapy staff members. I conducted my fieldwork in two stages, the first was exploratory so that I could build my understanding of the radiotherapy process, and the second was an in-depth and focused investigation into the patient experience.
Quantitative Questionnaire
I constructed a questionnaire to assay the patient experience of radiotherapy, looking closely at patient anxiety levels and their perceptions of the care environment. This method allowed me to generate statistically relevant information about the patient population being treated at NUS.
Design Probe Kits
I created and distributed design probe kits, containing a daily journal and disposable camera, to a small sub-section of patients for them to use to document their experiences as they went through radiotherapy. I received responses from 20 patients.
Synthesis
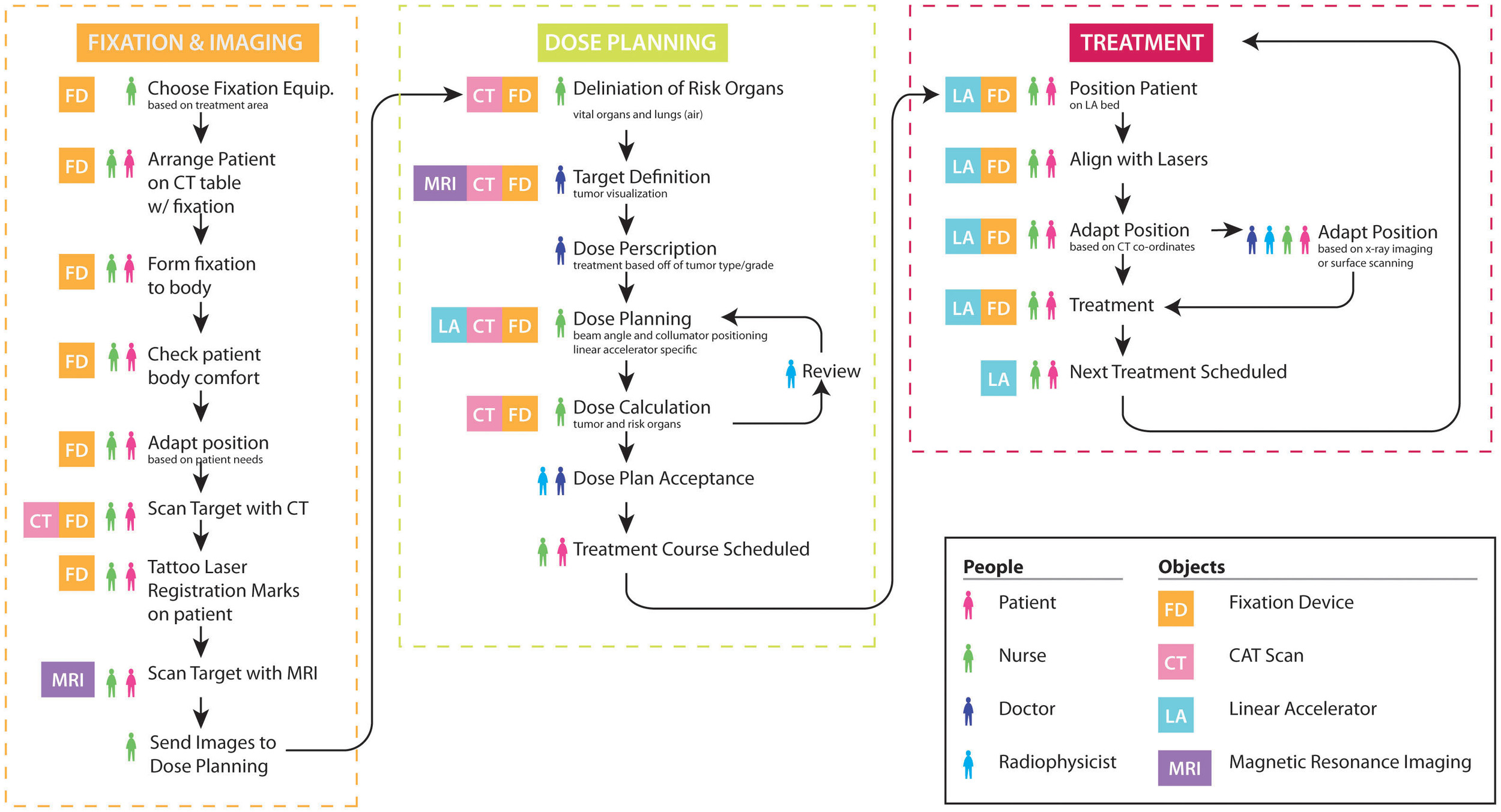
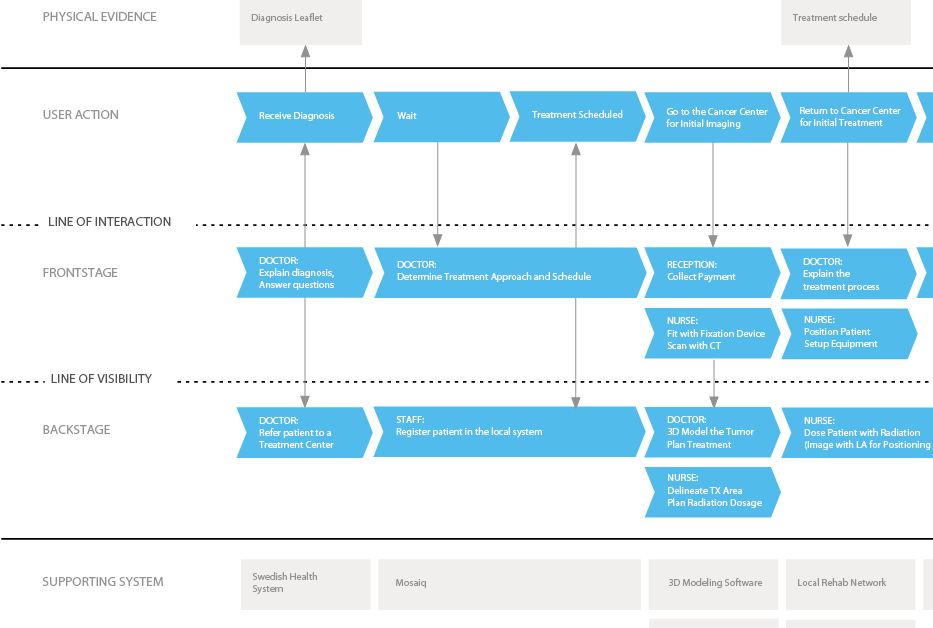
I used Service Design information mapping techniques to visualize the complex processes I observed during my fieldwork and help me process the information I had gathered about the radiotherapy workflow. I also used salience hierarchy to analyze my field notes, to look for commonalities and deviant occurrences within the patient experiences I had observed.
I thematically analyzed the material gathered from the patient journals and pictures in the design probe kits to identify the themes that were common across multiple patients’ experiences. I chose to focus my analysis upon the concrete examples of patient interactions within the treatment environment which elicited an emotional response from them.
I also looked for any significant relationships between the patients' experiences of the treatment environment and their anxiety levels by statistically analyzing the questionnaire data using SPSS (results published here).
Insights
Patients can experience situational anxiety as they go through radiotherapy. This complex emotion can be influenced by many factors, such as: worry over the medical equipment and feelings of isolation or claustrophobia during treatment.
Immobilization devices were designed to enable healthcare professionals to accurately position patients in a reproducible manner, but it does so by restraining the physical movement of the patient.
While the immobilization device has been designed in consideration for its use, operation, and management, its interactions with patients have generally been disregarded.
Design Directions
Based upon my research insights, I identified two possible design directions:
- To investigate whether a design intervention within the treatment environment could mediate some of the patient anxiety caused by the immobilization devices.
- To investigate if it would be possible to eliminate the need for immobilization devices if the patients became involved in the positioning process.
I decided to investigate both possibilities through the creation of experience prototypes that I could test with patients and the radiotherapy care staff.
Direction 1: Taklandskap
In my research, I found that many patients called attention to the lack of visual stimuli during their treatments. They even provided pictures of their view during treatment: ceiling tiles.
I decided to create a design that would alter the patient’s relationship with the treatment room environment in two ways. First, it would give them something to look at during treatment, and second, it would enable patients to actively customize the environment to their own personal preferences.
Experience Prototyping
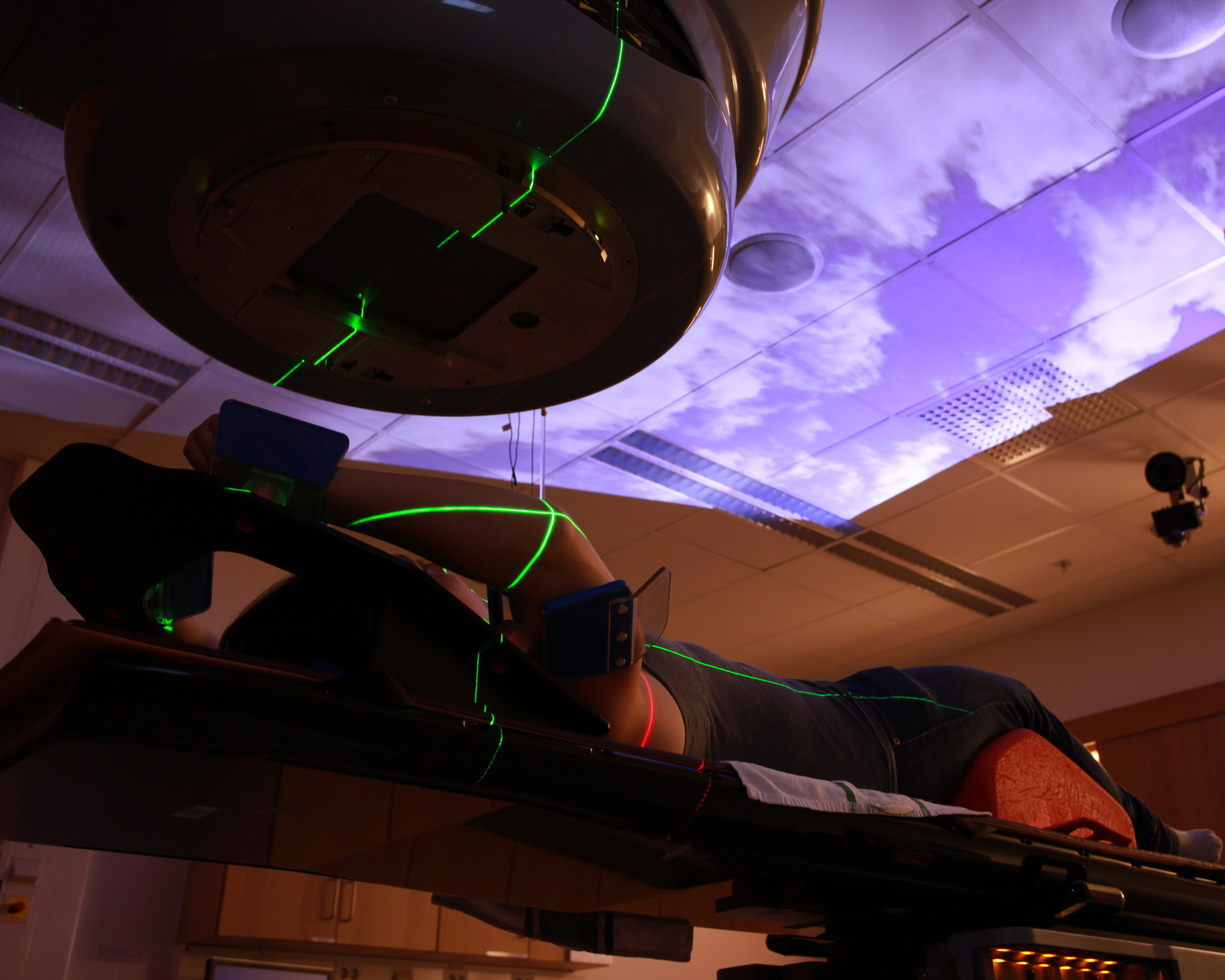
Working directly with the NUS radiotherapy staff to ensure that my design wouldn't interfere with their normal workflow, I developed a simple prototype using a DVD player and projector to display nature videos on the ceiling of the treatment room. The videos provided visual stimulation for patients, and a place to focus their attention during treatment. The prototype was installed in one of the treatment rooms in NUS’s Radiotherapy Department for initial testing.
Feedback about the prototype suggested that patients wanted to be able to choose what they could watch on the ceiling and also have sound/music playing with the videos.
I developed a second iteration of the prototype which included a touch screen interface where patients could choose what they wanted to watch and listen to during radiotherapy. I sketched out wireframes in Ai and build a fultional prototype in Flash using Actionscript3.
Implementation
The touch screen interface was installed within the two preparation rooms associated with the treatment room being used for the intervention. This enabled patients to select which music and video they would like to experience that day while they were preparing for their treatment. Once selected, the video was projected onto the ceiling of the treatment room, and the music was played through the room’s sound system.
Evaluation
The Taklandskap prototype was studied for its impact on the patient experience through a before/after comparison of the questionnaire data and design probe kits.
While statistical analysis of the questionnaire did not find that Taklandskap significantly decreased patient anxiety levels, patients reported that they enjoyed the intervention in their journals.
“It’s very nice and soothing to lie and look at the ceiling at all those beautiful pictures.”
”It’s an incredible experience. One forgets treatment and dreams away”
Direction 2: ActivPPS
The second experience prototype I developed attempted to remove the anxiety-causing immobilization device from the radiotherapy treatment process. In my research, I found that radiotherapy’s success is critically dependent upon the ability of a patient to be accurately repositioned into the same position for every treatment, and the radiotherapy staff are solely responsible for this positioning of the patient.
The patient is given no understanding of where their body is versus where it should be, and as a result, is completely dependent upon the radiotherapy staff to manually push, pull, and lift them into the correct position. I hypothesized that if the patient understood where their body should be, that they would be much more capable of moving their body into the correct position than the nurses.
I decided to create a system that would provide patients with the ability to visualize their body position in relation to the desired treatment position, and provide visual cues for when the two positions are correctly aligned.
Design Requirements
I began my prototyping process by mapping out the interactions that take place during patient positioning in radiotherapy, and used this to create a list of requirements for the self-positioning prototype. The prototype needed to be able to:
- Track the position of the body in real time and space
- Capture positional data about the body position at multiple points and in 3 dimensions
- Provide an output of this information in the form of visualizations and data
I chose to work with a Kinect™ sensor, because it can acquire 3D positional data and estimate the position of anatomical landmarks on the body in real time. These capabilities made it possible to create a concept prototype that tracked, visualized, and provided body position coordinates in a way that was accurate enough to test my patient positioning scenario.
Experience Prototyping
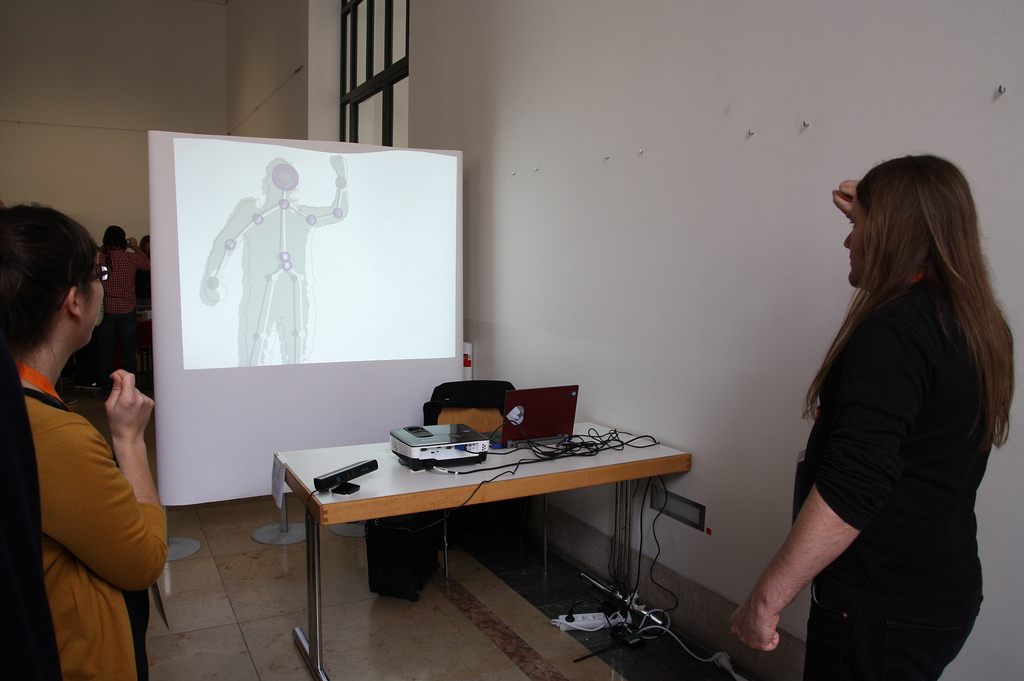
I sketched out the different interactions that I wanted the prototype to enable, and then worked with a software engineer to create a software prototype using the Microsoft SDK for the Kinect™ sensor that was able to recognize, visualize, track, and record the outline and skeleton of a person when they are moving in front of the sensor.
Sketch of how the active and recorded positional data could be visualized.
A. Active skeleton (blue) being transformed into recorded positional data (grey).
B. Overlap of the active and recorded skeletons.
C. Correct alignment of four joints noted by the halos.
While the prototype, named ActivPPS, could not be implemented within NUS’s radiotherapy department because it disrupted radiotherapy’s highly regulated treatment processes, it was constructed so that individuals could interact with it.
Evaluation
I tested ActivPPS prototype in a series of workshops and discussions with designers and radiotherapy experts to evaluate its feasibility and assess the potential change to patient experience by shifting their role in the radiotherapy positioning process from passive to interactive.
Through this dialogue, it became clear that while the ActivPPS prototype could be extremely useful for engaging patients in the positioning process, it could not replace the fixation device without putting unnecessary stress on the patient because they would become solely responsible for maintaining their position for a long duration of time without support
Despite this, the prototype received a positive reception from the Swedish Test-bed for Innovative Radiotherapy as a tool that would allow both the patient and the radiotherapy nurses to work together through mutually-supportive interactions to achieve correct alignment.
Shifting the roles of the patient (blue) and nurse (grey) within the radiotherapy positioning process.
Impact
Taklandskap has become a permanent installation within the treatment room at NUS. The design assets have been transferred to the Radiotherapy Department so that they can maintain the design, and they are working to install the system in additional treatment rooms.
ActivPPS has received support from the Swedish innovation financier, Vinnova, to fund further development of the technology so that it can be tested within the clinical environment.